Imagine preparing for a marathon. You wouldn’t just show up on race day, right? You’d train, fuel your body, and have a solid plan for recovery afterward. Well, modern surgery isn’t so different. That’s the core idea behind Enhanced Recovery After Surgery (ERAS) protocols. They’re the comprehensive training and recovery plan for your body’s biggest physical challenge.
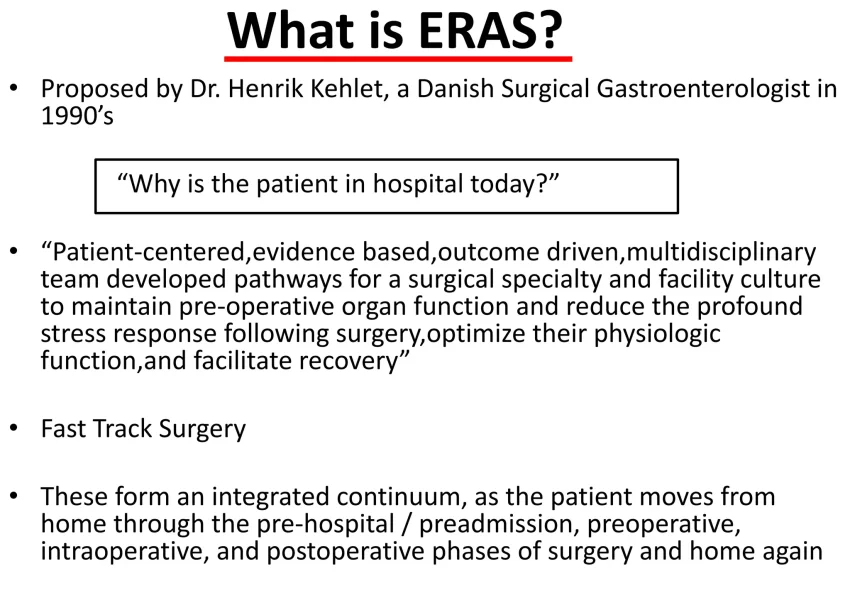
Honestly, ERAS flips the old script on its head. Gone are the days of prolonged fasting, routine drains and tubes, and bedrest being the default. Instead, these evidence-based pathways are a multidisciplinary cocktail of best practices—spanning from before admission to after discharge—designed to reduce surgical stress, manage pain with less opioids, and get you back on your feet, faster and safer.
The Common Threads: What Makes an ERAS Protocol Tick
While tailored to each operation, all successful ERAS pathways share a common DNA. Think of them as having three key phases: prehabilitation, intraoperative care, and post-operative recovery. The goal? To maintain your body’s normal function as much as possible.
Preoperative Phase: Setting the Stage
This is where the groundwork is laid. Key elements here include:
- Patient Education & Expectation Management: Knowing what to expect reduces anxiety, which honestly is a huge pain trigger.
- Nutritional Optimization: We’re screening for malnutrition and sometimes using carbohydrate-loaded drinks up to 2 hours before surgery—it’s like topping off your fuel tank.
- Prehabilitation: Simple exercises, quitting smoking, and managing chronic conditions. It’s about building physiological reserve.
Intraoperative & Postoperative: The Active Steps
Here’s the deal: during and after surgery, the focus shifts to minimizing insult and promoting mobility. That means:
- Multimodal, opioid-sparing pain control (using several different types of pain meds).
- Goal-directed fluid therapy—giving just the right amount of IV fluids, not flooding the system.
- Preventing nausea and vomiting proactively.
- And perhaps most famously, getting patients out of bed and eating a normal diet on the same day as surgery in many cases.
ERAS in Action: A Cross-Specialty Tour
The beauty of ERAS is its adaptability. Let’s look at how these principles are applied across different surgical fields. You’ll see the common themes, but also the specialty-specific nuances that make all the difference.
Colorectal Surgery: The Pioneer
ERAS was practically born here. For bowel surgeries, the protocols are robust and well-studied. A major shift? Moving away from harsh mechanical bowel prep, which can dehydrate and stress patients. Instead, the focus is on minimal fasting and early reintroduction of diet to get the gut working again. The results are impressive—reducing complications and slashing length of stay by days.
Orthopedic Surgery (Joint Replacement)
For hip and knee replacements, ERAS is a game-changer. It’s all about managing pain and mobilizing fast. That involves regional nerve blocks (numbing just the surgical limb), tranexamic acid to reduce blood loss, and a fierce commitment to physical therapy starting just hours after surgery. The aim isn’t just to leave the hospital sooner, but to achieve functional independence rapidly.
Gynecologic & Urologic Surgery
In surgeries like hysterectomies or prostatectomies, ERAS pathways emphasize minimizing opioid use—which can cause constipation and urinary retention, two big post-op issues in these specialties. They also prioritize early removal of catheters and, you know, getting back to a normal diet to help the body’s systems reset.
| Surgical Specialty | ERAS Focus Areas | Key Outcome Goals |
| Colorectal | Gut function, no routine drains, early feeding | Reduce ileus, infections, length of stay |
| Orthopedic (Joints) | Multimodal pain control, blood management, immediate PT | Rapid functional recovery, reduce blood transfusions |
| Cardiothoracic | Early extubation, strict fluid balance, glycemic control | Reduce pulmonary complications, atrial fibrillation |
| Hepatobiliary | Nutritional support, meticulous fluid management | Prevent liver failure, reduce infections |
The Real-World Hurdles & Why They Matter
Implementing ERAS isn’t always a smooth ride. It requires a cultural shift. Surgeons, anesthesiologists, nurses, physiotherapists, and dietitians all have to row in the same direction. Old habits—like keeping a patient “NPO after midnight” or defaulting to opioid PCA pumps—can be tough to break.
Another pain point? Patient variability. A one-size-fits-all protocol doesn’t exist. The art is in adapting the framework to the individual—the 80-year-old with multiple conditions versus the otherwise healthy 40-year-old. That’s where clinical judgment and the “enhanced” part of recovery truly live.
The Bottom Line: A New Philosophy of Care
So, what are we left with? Enhanced Recovery After Surgery protocols represent more than a checklist. They signal a fundamental shift from a passive, “let’s wait and see” model to an active, physiological-preservation model. It’s about respecting the body’s innate capacity to heal when we remove the unnecessary obstacles we used to put in its way.
The data is compelling across specialties—fewer complications, shorter hospital stays, better patient experiences, and often, lower costs. But maybe the most profound impact is intangible: it gives patients a sense of agency and partnership in their own recovery. They’re not just a surgical site; they’re an active participant in the marathon. And that changes everything.